Leaving Blue Cross Blue Shield of Arizona
Pressing “Continue” takes you outside of azblue.com, which is not controlled by Blue Cross Blue Shield of Arizona.
Population Health | Care Coordination
Care coordination for optimal outcomes
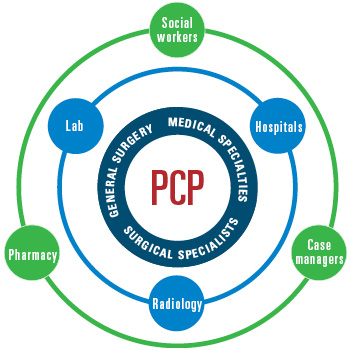
Care coordination is the result of deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient's care to achieve safer and more effective care. This means that the patient's needs and preferences are known ahead of time and communicated at the right time to the right people, and that this information is used to provide safe, appropriate, and effective care to the patient.*
* Source of definition: Agency for Healthcare Research and Quality (AHRQ)
Learn more about care coordination.
Actions for BCBSAZ network providers
Effective care coordination includes the following actions:
- Provide coordination of care for patients with complex conditions.
- Refer members to in-network specialists.
- Follow up with patients for compliance with specialist care plan.
- Assess barriers to compliance and care, and intervene as needed.
- Coordinate medical team conferences between specialists and PCP.
- Reduce duplication of services (lab, radiology across PCP and specialists).
- Address co-morbidities including behavioral health issues.
- Provide proactive follow up post admission.
- Call member to schedule a 7-day follow up appointment.
- Perform medication reconciliation.
- Review any notifications that have been sent to you about gaps in care for your
BCBSAZ patients.
- Assess potential care gaps.
- Schedule patient appointments, tests, and follow-up as needed to close gaps.
- Document condition persistency to facilitate appropriate claim coding for each patient
encounter.
- Schedule annual appointments with patients to review medical plan.
- Refer members to BCBSAZ HealthyBlue programs for wellness and care management.
BCBSAZ Care Management Program
For members with persistent health conditions, clinically-trained BCBSAZ Care Managers collaborate with providers in addressing special needs for patient care to augment the physician care management.
The URAC-accredited BCBSAZ Care Management Program assists in managing a member's complex, catastrophic or chronic healthcare needs through appropriate resources to promote wellness, prevention, and positive health outcomes across the continuum of care.
Concerned about a BCBSAZ member? Call us at (877) 694-2583
![]()
Access the BCBSAZ Care Management Referral Form.
BCBSAZ Transition of Care Program
The BCBSAZ Transition of Care Program partners with hospitals to decrease preventable readmissions through strategic telephonic interactions to support medication adherence and PCP follow-up. Members with multiple admissions are targeted for this program.
- Goals:
- Lower hospital readmission rates
- Maximize care coordination
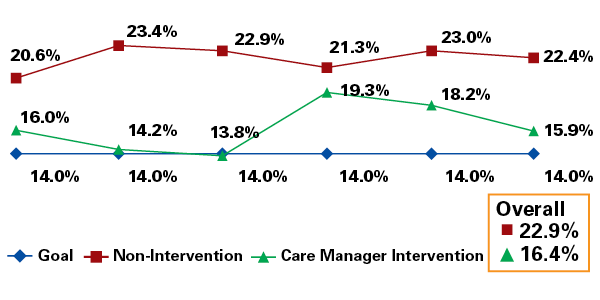
RESULTS—Readmission Rates for a New Diagnosis (2011-2013)
HealthyBlue Health and Wellness Programs
The BCBSAZ HealthyBlue Program is an integrated program of health and wellness tools designed to support providers with effective care coordination. This program consists of resources and services geared toward educating, engaging and empowering members to make healthier lifestyle choices.
For a complete list and specific information about each of the tools, access the provider HealthyBlue webpage. Several HealthyBlue services are available to all members. Other programs and services depend on the member's plan type and personal circumstances. Some of the HealthyBlue services are provided through independent contractors.*
* PLEASE NOTE: Independent contractors who offer some HealthyBlue programs are not affiliated with BCBSAZ and are solely responsible for the services and/or products offered.
Additional Resources
Want more information? The Agency for Healthcare Research and Quality website has excellent care coordination resources that may be helpful in developing systems for effective care.